More Support Needed to Maintain Strides Made by Community Health Centers
COMMENTARY
As the impact of the omicron variant of COVID-19 appears to wane, the U.S. is entering the third year of the pandemic and its disruptions are a fact of life in the fabric of our daily lives. The trouble is, we have less psychological reserve with which to respond to these challenges.
This is especially true for the health care industry which had well-documented, pre-COVID challenges with staff well-being and vacancies.
The American Nurses’ Association has called on the federal government to declare our current nursing shortage a national crisis, and reports of attacks on vaccine sites in New York and California underscore the perils we face.
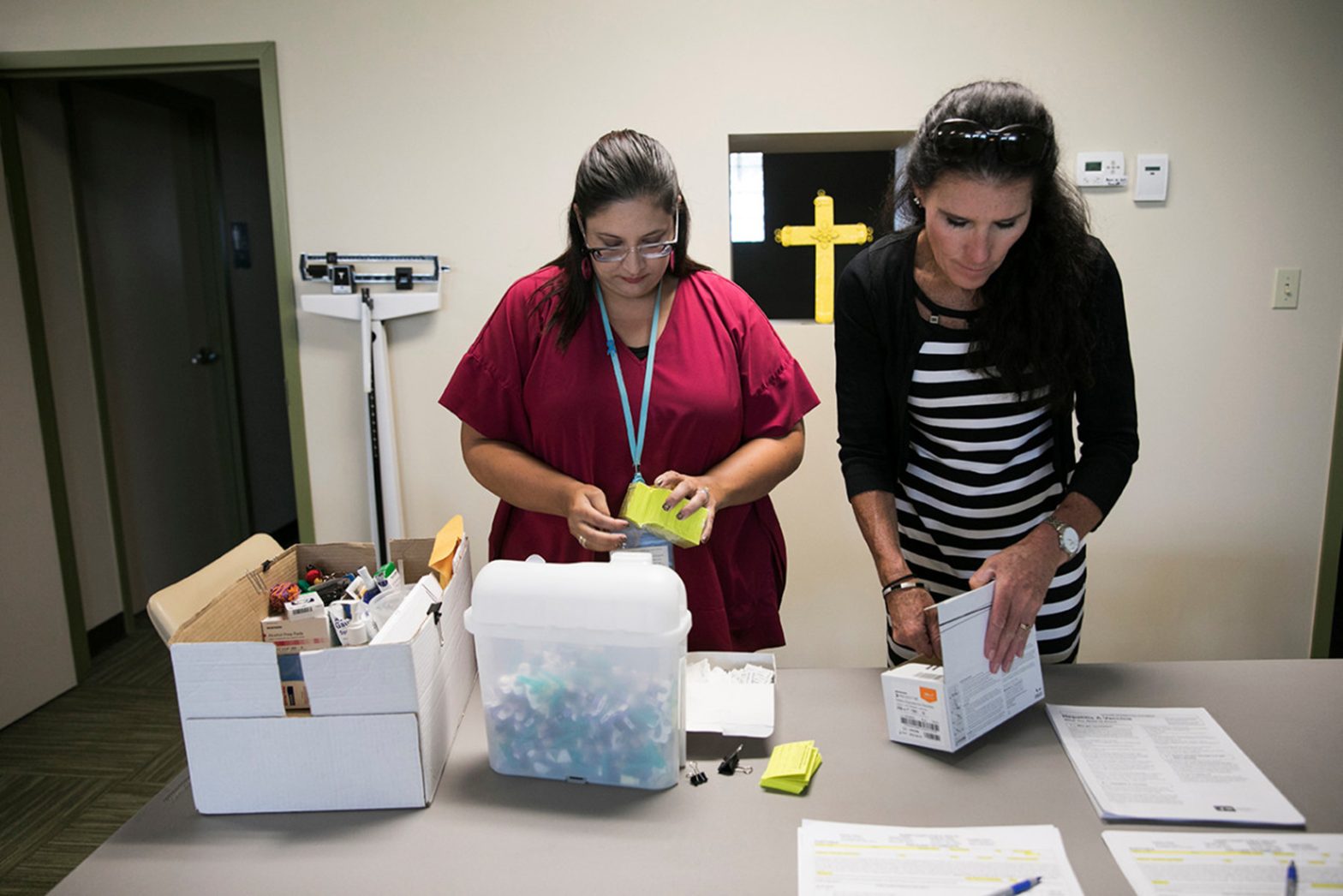
Community Health Centers, also known as Federally Qualified Health Centers, which provide quality, comprehensive primary care and other medical and behavioral health services to the nation’s most vulnerable patients, are all too familiar with workforce shortages.
By statute and design they are located in federally designated Health Professional Shortage Areas, and are frequently unable to match provider and staff wages and benefits offered by large health care systems.
A workforce report by the National Association of Community Health Centers highlights the “immense strain” put on these health center workers, and calls consistent federal investments in primary care workforce programs “essential” to their success.
The National Health Service Corps offers student loan repayment for physicians and other members of the primary care team who commit to working in HPSAs upon completion of their training.
It is not uncommon for doctors to accumulate half a million dollars in loan debt before they finish residency. Relief from debt burden through the National Health Service Corps enables them to work as health center primary care providers.
In November 2021 the National Health Service Corps, the Nurse Corps and the Substance Use Disorder Treatment and Recovery Loan Repayment programs received an infusion of $1.5 billion in additional federal funding to address health care workforce shortages in underserved communities. The programs also provided scholarships and loan repayment for nurses, primary care and behavioral health providers.
Dr. Jae Ahn, D.O., chief medical officer at Union Community Health Center in New York, says the corps has been “very helpful” in attracting providers to work there. If it did not exist, “you would have many fewer candidates to work in underserved areas. I would probably have half the workforce,” said Ahn.
Community Health Centers have responded to health care disparities that have been worsened by the pandemic. Responding to the health and well-being of fully staffed teams is essential to our ability to continue this vital work. Additional federal dollars are needed to address shortages of health care workers in underserved communities.
Congress should prioritize allocating resources to programs like the Teaching Health Center Graduate Medical Education Program, the National Health Service Corps and the Nurse Corps Loan Repayment Program, all of which will broaden the workforce pipelines health centers depend on to provide care to patients.
Dr. Grace Wang is a family physician and a senior fellow of Public Health Integration and Innovation at the National Association of Community Health Centers. Dr. Wang spent more than 30 years working at health centers and public health departments in New York City, New York, and Seattle, Washington, most recently at International Community Health Services in Seattle. In addition to providing primary care, Dr. Wang has also served as health center teaching faculty for ARNP and family medicine residents as well as in clinical leadership roles as medical director and chief medical officer. Dr. Wang graduated from the University of Michigan with a degree in Early Childhood Education. She received her medical training at Cornell University Medical College (now Weill Cornell Medicine) in New York City and has a master’s degree in Public Health, also from the University of Michigan.
You can find the National Association of Community Health Centers on Twitter @NACHC.























