Bacterial Spores Inspire Novel Cancer Drug Delivery System
WASHINGTON — Scientists with the National Cancer Institute’s Center for Cancer Research have come up with a new way to get life-saving drugs directly into cancer cells, an advance they say will enable more effective treatments for cancer with fewer side effects.
The research was originally published in Cell Reports.
As noted in a press release from the agency, the side effects of some chemotherapy drugs can range from nausea and fatigue to mood changes and nerve problems, as well as damage to healthy cells and organs.
“These side effects are a huge deterrent for people getting chemotherapy,” said Kumaran Ramamurthi, Ph.D., senior investigator and deputy chief of the Laboratory of Molecular Biology, in a written statement.
Ramamurthi, who was also lead investigator of the study, went on to say, “One way to solve this problem is to make sure that chemotherapy drugs reach only the cancer and not surrounding tissue.”
Ramamurthi’s team created artificial, bacterial spore-like particles that can target cancer while carrying chemotherapeutic cargo.
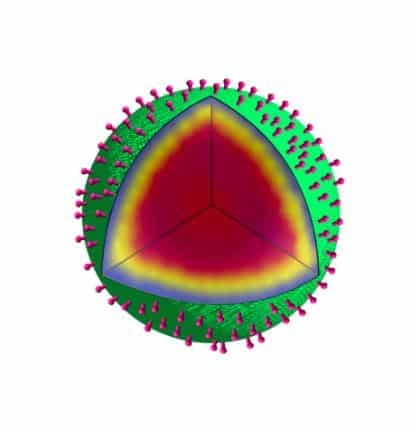
The product, called a SSHEL (short for Synthetic Spore Husk-Encased Lipid bilayers), consists of a porous glass bead surrounded by a membrane and a protein coat dotted with cancer-targeting molecules.
To test their concept, the team collaborated with the groups headed by David Fitzgerald, Ph.D., senior investigator in the Laboratory of Molecular Biology, and Kandice Tanner, Ph.D., senior investigator in the Laboratory of Cell Biology, to use a mouse model of HER2-positive ovarian cancer, which is sometimes treated with a chemotherapy drug called doxorubicin.
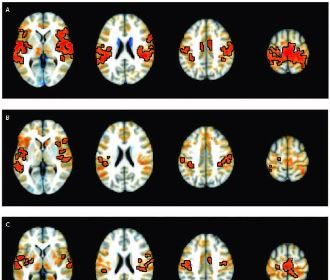
They loaded doxorubicin into SSHELs designed to home in on HER2 proteins and then injected the SSHELs into the mice. Compared to the leading doxorubicin delivery method (doxorubicin encased in a fat-based sphere), the SSHELs shrank the tumors more effectively and with fewer side effects, the release said.
In a serendipitous twist, it was the cancer cell’s own machinery that secured its demise. The team’s initial goal was to reach the cancer and then work on drug release, but when the SSHELs contacted the cancer cell surface, they were trafficked into an acidic area of the cell. This destabilized the SSHEL particle and released the doxorubicin cargo.
“That was unexpected, but it was fortuitous,” Ramamurthi said.
The team confirmed their findings in a transparent zebrafish model of ovarian cancer. Using fluorescent markers, they tracked the SSHELs at the surface of cancer cells and inside acidic compartments.
Ramamurthi and collaborators plan to examine the utility of SSHELs in another mouse model, but he emphasized in a written statement that the relevance of SSHEL extends far beyond ovarian cancer and chemotherapeutic drug delivery.
“We’re providing a versatile platform that could be used for a lot of different applications. Tell us what should be targeted, and we could provide a vehicle to get the cargo there,” he said.
Dan can be reached at [email protected] and at https://twitter.com/DanMcCue