Millions Could Lose Medicaid Coverage Following End of PHE
WASHINGTON — The federal COVID-19 public health emergency, first declared Jan. 27, 2020, was set to expire on April 16. Health and Human Services Secretary Xavier Becerra on Wednesday extended the COVID-19 public health emergency for 90 days.
A number of health policy experts have been raising concerns about what end of the public health emergency could mean for Medicaid beneficiaries.
“States have gotten extra federal funding and in return have not been able to disenroll anyone involuntarily. When the PHE lifts the funding will go away and states will have a year to process renewals for everyone on Medicaid. This is a huge task and many states are understaffed,” said Joan Alker, executive director at the Center for Children and Families, Georgetown University McCourt School of Public Policy in an email to The Well News.
The 90-day extension would end the PHE in mid-July, and the U.S. Department of Health and Human Services has agreed to issue a 60-day notice prior to the expiration of the PHE emergency.
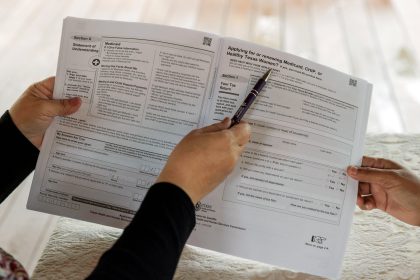
Under the Families First Coronavirus Response Act, passed in 2020, Medicaid agencies were prohibited from disenrolling beneficiaries until the end of the month in which the public health emergency expires.
The Urban Institute estimates that nearly 15 million people may lose Medicaid coverage because they do not qualify after the end of the PHE.
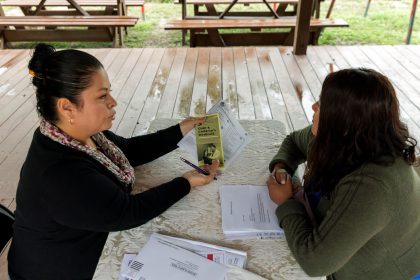
“Lots of kids and families lose Medicaid coverage routinely due to what we call procedural denials. A renewal letter gets lost in the mail, and the family loses coverage or fails to complete the renewal process. [Often] because they are homeless or have limited English language skills. These ‘red tape’ losses happen all the time but the pandemic has avoided them, and likely this provision prevented the uninsured rate from going up during a pandemic,” said Alker.
“Congress could step in and set a date [certain] at least for the Medicaid provisions,” said Alker, in her recommendations.
A report was recently released from researchers at the Center for American Progress which examines how state and federal policymakers can prevent disruptions to coverage and care for millions of Medicaid enrollees facing disenrollment and preserve critical access to testing and treatment.
“CMS released two pieces of guidance, one at the end of 2021, and another piece of guidance at the beginning of March. The latest guidance … provides states with a longer runway once the public health emergency is over to complete redetermining all of their Medicaid eligibility,” said Natasha Murphy, lead author of the report and director of Health Policy at the Center for American Progress, during a phone call with The Well News.
Murphy said states were originally given 12 months after the expiration of the public health emergency to make Medicaid redeterminations, but the latest CMS guidance extends this to 14 months and includes recommendations for states in making redeterminations.
“There is the expectation that HHS will renew the declaration for another 90 days, but states have indicated they need as much leeway time as possible to firm up and finalize,” said Murphy.
“[In the report] we call for a 120-day notification… We are already in that window. [We need] a clear statement from HHS as soon as possible as to whether they renew the PHE beyond July,” continued Murphy.
According to Murphy, the HHS said it would be difficult to give lengthy advance notice of the end of the PHE, and that the agency can do so only in 90-day increments.
This is why it is important for states to be aware of what is feasible for their emergency measures to protect their citizens, according to Murphy.
The report also explores ways in which states can leverage the number of relief funds received through things like the American Rescue Plan.
“There is the opportunity for states to attempt innovative studies at the state-level [with those relief funds] to advance public health and health care,” said Murphy.
Among other things, the FFCRA and Coronavirus Aid, Relief, and Economic Security Act also required state Medicaid programs to cover COVID-19 testing, vaccination, and treatment with no cost sharing through the last day of the first quarter after the end of the public health emergency.
Murphy said Congress should take immediate action to pass a bill that includes emergency funding for the continuation of the COVID-19 uninsured fund.
“The uninsured fund has essentially been tapped. There is no reimbursement left for uninsured individuals… for their PCR testing, as well as vaccine administrative costs … but the pandemic is not quite over yet,” said Murphy.
Alexa can be reached at [email protected]