KFF Details COVID’s Effect on State Medicaid in Latest Report

WASHINGTON — COVID-19 has had a profound impact on the finances, ongoing operations and priorities of state Medicaid programs, according to a new report released by the Kaiser Family Foundation.
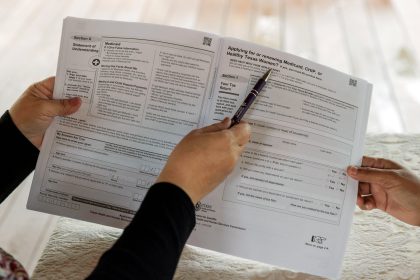
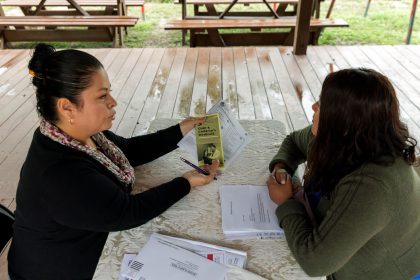
Responses from the survey, which the nonprofit has conducted annually for 22 years, show changes in state Medicaid enrollment numbers, spending trends and assumptions about the end of the pandemic.
Findings from KFF’s new state Medicaid budget survey, answered by 49 states, show that officials anticipate an end to the public health emergency in 2023, which will lead to Medicaid enrollment declines, slower total Medicaid spending growth and likely a sharp rise in states’ share of costs.
“Early in the pandemic, the Families First Coronavirus Response Act included requirements for states to provide continuous coverage for Medicaid enrollees in exchange for enhanced federal matching funds,” Robin Rudowitz, vice president and director for Program on Medicaid and the Uninsured, shared at an event to release report findings.
“These provisions have helped to ensure stable coverage for Medicaid enrollees and to provide substantial fiscal relief to states.”
But with these requirements and boosted funds expected to end in early 2023, states are set to restart Medicaid qualifications.
And Medicaid officials have reported that uncertainties related to the end of the public health emergency make it difficult to plan and develop state budgets.
“No doubt the public health emergency unwinding will be the predominant issue for the foreseeable future,” Dianne Hasselman, interim executive director for the National Association of Medicaid Directors, said.
“States are as prepared as they can be … crouched and ready at the starting line. But the state agency workforce has been significantly compromised; Congress is a wild card in all of this and could make decisions before the end of the year that might undercut the planning and preparation that states have been doing.”
State Medicaid officials expect enrollment declines that are likely to accelerate over time, but state spending growth is projected to increase, not only because the federal funds boost will sunset, but due to inflationary pressures, increased service utilization, and increased home and community-based services spending.
Still, state Medicaid directors say they are trying to keep up the momentum of the public health emergency to make structural changes to their programs.
This is because the pandemic has shaped states’ Medicaid policy priorities — or highlighted the urgency of work started before the public health emergency took effect.
A companion report to KFF’s budget survey shows that while states continue to respond to pandemic-related health issues such as increasing vaccination and booster rates and treating long-COVID, they are sharply focusing on reducing disparities, preserving telehealth and enhancing access to behavioral health services.
“More states are adding or expanding covered benefits than making cuts,” Libby Hinton, associate director for Program on Medicaid and the Uninsured, explained.
Areas of benefit expansion include preventive services, dental services, pregnancy and postpartum services, and services to address enrollees’ social needs like food and housing.
Telehealth is also likely to remain an area of active policy development in the coming years, as most states have or plan to adopt permanent Medicaid telehealth policy expansions that will remain in place even after the pandemic.
But of course, any of this could change with the result of upcoming gubernatorial elections and as inflation and other factors shift political and fiscal landscapes.
As Kathy Gifford, principal for Health Management Associates, said, “As always, it is an exciting and challenging time to serve as a Medicaid director.”
Kate can be reached at [email protected]